James Sikes, M.D.
- Home
- Physicians
- James Sikes, M.D.

James Sikes was born the youngest of 4 children in Saraland, Alabama. His mother worked as a medical technologist and his father, who was a World War II veteran, was a dentist. After attending high school in Mobile, Ala, he attended the University of Mississippi on an athletic scholarship. Following his undergraduate education he attended medical school at the University of Alabama Birmingham.
During medical school at UAB he performed research in total joint replacement at the Andrew’s South Highland Hospital and worked with local orthopedic surgeons. This experience led him to the orthopedic surgery training program in Jackson, MS, led by Dr. James Hughes and Dr. Bob McGuire. During his residency he chose a sabbatical in Jackson, Wyoming for further training in trauma and sports medicine.
After practicing for four years in Brookhaven, he joined Southern Bone and Joint Specialists in 2002. During Dr. Sikes’ years of service the practice has expanded to include the development of the Orthopedic Institute.
One of the unique offerings of Dr. Sikes’ practice is Bilateral Knee Replacement.

-
Direct Phone Number
(601) 543-7257
Robotic Assisted Surgery/Makoplasty
Over the years, joint replacement techniques and instrumentation have undergone countless improvements. Mako Technology is designed to help surgeons provide patients with a personalized surgical experience based on their specific diagnosis and anatomy.
- Mako Robotic-Arm Assisted Technology for Total Hip Replacement
- Mako Robotic-Arm Assisted Technology for Partial Knee Replacement
- Mako Robotic-Arm Assisted Technology for Total Knee Replacement
Services
-
Arthritis
Arthritis
The term arthritis literally means inflammation of a joint, but is generally used to describe any condition in which there is damage to the cartilage. Inflammation is the body’s natural response to injury. The warning signs that inflammation presents are redness, swelling, heat and pain.
The cartilage is a padding that absorbs stress. The proportion of cartilage damage and synovial inflammation varies with the type and stage of arthritis. Usually the pain early on is due to inflammation. In the later stages, when the cartilage is worn away, most of the pain comes from the mechanical friction of raw bones rubbing on each other.
There are over 100 different types of rheumatic diseases. The most common are:
Osteoarthritis: Osteoarthritis is also called as degenerative joint disease; this is the most common type of arthritis, which occurs often in older people. This disease affects cartilage, the tissue that cushions and protects the ends of bones in a joint. With osteoarthritis, the cartilage starts to wear away over time. In extreme cases, the cartilage can completely wear away, leaving nothing to protect the bones in a joint, causing bone-on-bone contact. Bones may also bulge, or stick out at the end of a joint, called a bone spur.
Osteoarthritis causes joint pain and can limit a person’s normal range of motion (the ability to freely move and bend a joint). When severe, the joint may lose all movement, causing a person to become disabled. Disability most often happens when the disease affects the spine, Knees, and Hips.
Rheumatoid Arthritis: This is an auto-immune disease in which the body’s immune system (the body’s way of fighting infection) attacks healthy joints, tissues, and organs. Occurring most often in women of childbearing age (15-44), this disease inflames the lining (or synovium) of joints. It can cause pain, stiffness, swelling, and loss of function in joints. When severe, rheumatoid arthritis can deform, or change, a joint. For example, the joints in a person’s finger can become deformed, causing the finger to bend or curve.
Rheumatoid Arthritis affects mostly joints of the hands and feet and tends to be symmetrical. This means the disease affects the same joints on both sides of the body (both the hands or both feet) at the same time and with the same symptoms. No other form of arthritis is symmetrical. About two to three times as many women as men have this disease.
Post-traumatic arthritis: Arthritis developing following an injury to hand, wrist or elbow is called as post-traumatic arthritis. The condition may develop years after the trauma such as a fracture, severe sprain, or ligament tears.
Psoriatic arthritis: This form of Arthritis occurs in some persons with psoriasis, a scaling skin disorder, affecting the joints at the ends of the fingers and toes. It can also cause changes in the fingernails and toenails. Back pain may occur if the spine is involved.Causes of Arthritis
Osteoarthritis is caused by the wearing out of the cartilage covering the bone ends in a joint. This may be due to excessive strain over prolonged periods of time, or due to other joint diseases, injury or deformity. Primary osteoarthritis is commonly associated with ageing and general degeneration of joints.
Secondary osteoarthritis is generally the consequence of another disease or condition, such as repeated trauma or surgery to the affected joint, or abnormal joint structures from birth.
Rheumatoid arthritis is often caused when the genes responsible for the disease is triggered by infection or any environmental factors. With this trigger body produce antibodies, the defense mechanism of body, against the joint and may cause rheumatoid arthritis.
Fractures at joint surfaces and joint dislocations may predispose an individual to develop post-traumatic arthritis. It is considered that your body secretes certain hormones following injury which may cause death of the cartilage cells.
Uric acid crystal build-up is the cause of gout and long-term crystal build-up in the joints may cause deformity.Symptoms of Arthritis
There are more than 150 different forms of arthritis. Symptoms vary according to the form of Arthritis. Each form affects the body differently. Arthritic symptoms generally include swelling and pain or tenderness in one or more joints for more than two weeks, redness or heat in a joint, limitation of motion of joint, early morning stiffness, and skin changes including rashes.
Diagnosis
Doctors diagnose arthritis with a medical history, physical exam and X-rays of the affected part. Computed tomography (CT) scans and magnetic resonance imaging (MRI) scans are also performed to diagnose arthritis.
Treatment Options
There is no cure for arthritis. Your doctor may prescribe anti-inflammatory medicine. They may recommend occupational therapy or physiotherapy, which includes exercises and heat treatment. In severe cases, surgery may be suggested. The type of surgery will depend on your age and severity of the disease. In the elderly with severe arthritis, joint replacement can give good results.
Initial treatment for arthritis is conservative, consisting of rest, avoidance of vigorous weight bearing activities, and the use of non-narcotic analgesic and/or anti-inflammatory medications. With worsening symptoms a cane or braces may be helpful. For more severe symptoms, an injection of cortisone into the joint is frequently advised and can be quite helpful. When conservative measures have been exhausted, offer no relief, and has become disabling, the surgery may be recommended. Surgery is usually considered if nonsurgical treatment fails to give relief. There are different surgical procedures that can be used and may include:
Synovectomy: This surgery is usually indicated for early cases of inflammatory arthritis where there is significant swelling (synovitis) that is causing pain or is limiting the range of motion. Synovectomy is a surgical removal of the inflamed synovium (tissue lining the joint). The procedure may be performed using arthroscopy.
Arthroplasty: In this procedure, your surgeon removes the affected joint and replaces it with an artificial implant. It is usually performed when the joint is severely damaged by osteoarthritis, rheumatoid arthritis, post-traumatic arthritis or avascular necrosis. The goal of the surgery is to relieve pain and restore the normal functioning of the joint. Total joint replacement can be performed through an open or minimally invasive approach.
Arthrodesis: A fusion, also called an arthrodesis involves removal of the joints and fusing the bones of the joint together using metal wires or screws. This surgery is usually indicated when the joints are severely damaged, when there is limited mobility, damage to the surrounding ligaments and tendons, failed previous arthroplasty, and when heavy manual use is expected.
Your surgeon will discuss the options and help you decide which type of surgery is the most appropriate for you. -
Knee
- Normal Anatomy of the Knee Joint
- Knee Fracture
- Meniscus Tear
- Mako Robotic-Arm Assisted Technology for Partial Knee Replacement
- Mako Robotic-Arm Assisted Technology for Total Knee Replacement
- Patellofemoral Instability
- Knee Osteoarthritis
- Total Knee Replacement (TKR)
- Ligament Reconstruction
Normal Anatomy of the Knee Joint
The knee is made up of four bones. The femur or thighbone is the bone connecting the hip to the knee. The tibia or shinbone connects the knee to the ankle. The patella (kneecap) is the small bone in front of the knee and rides on the knee joint as the knee bends. The fibula is a shorter and thinner bone running parallel to the tibia on its outside. The joint acts like a hinge but with some rotation.
The knee is a synovial joint, which means it is lined by synovium. The synovium produces fluid lubricating and nourishing the inside of the joint. Articular cartilage is the smooth surfaces at the end of the femur and tibia. It is the damage to this surface which causes arthritis.
Femur - The femur (thighbone) is the largest and the strongest bone in the body. It is the weight bearing bone of the thigh. It provides attachment to most of the muscles of the knee.
Condyle - The two femoral condyles make up for the rounded end of the femur. Its smooth articular surface allows the femur to move easily over the tibial (shinbone) meniscus.
Tibia - The tibia (shinbone), the second largest bone in the body, is the weight bearing bone of the leg. The menisci incompletely cover the superior surface of the tibia where it articulates with the femur. The menisci act as shock absorbers, protecting the articular surface of the tibia as well as assisting in rotation of the knee.
Fibula - The fibula, although not a weight bearing bone, provides attachment sites for the Lateral collateral ligaments (LCL) and the biceps femoris tendon.
The articulation of the tibia and fibula also allows a slight degree of movement, providing an element of flexibility in response to the actions of muscles attaching to the fibula.
Patella - The patella (kneecap), attached to the quadriceps tendon above and the patellar ligament below, rests against the anterior articular surface of the lower end of the femur and protects the knee joint. The patella acts as a fulcrum for the quadriceps by holding the quadriceps tendon off the lower end of the femur.
Menisci - The medial and the lateral meniscus are thin C-shaped layers of fibrocartilage, incompletely covering the surface of the tibia where it articulates with the femur. The majority of the meniscus has no blood supply and for that reason, when damaged, the meniscus is unable to undergo the normal healing process that occurs in the rest of the body. The menisci act as shock absorbers, protecting the articular surface of the tibia as well as assisting in rotation of the knee. As secondary stabilizers, the intact menisci interact with the stabilizing function of the ligaments and are most effective when the surrounding ligaments are intact.
Anterior Cruciate Ligament (ACL) - The anterior cruciate ligament (ACL) is the major stabilizing ligament of the knee. The ACL is located in the center of the knee joint and runs from the femur (thigh bone) to the tibia (shin bone), through the center of the knee. The ACL prevents the femur from sliding backwards on the tibia (or the tibia sliding forwards on the femur). Together with the posterior cruciate ligament (PCL), ACL stabilizes the knee in a rotational fashion. Thus, if one of these ligaments is significantly damaged, the knee will be unstable when planting the foot of the injured extremity and pivoting, causing the knee to buckle and give way.
Posterior Cruciate Ligament (PCL) - Much less research has been done on the posterior cruciate ligament (PCL) because it is injured far less often than the ACL. The PCL prevents the femur from moving too far forward over the tibia. The PCL is the knee’s basic stabilizer and is almost twice as strong as the ACL. It provides a central axis about which the knee rotates.
Collateral Ligaments - Collateral Ligaments prevent hyperextension, adduction, and abduction- Superficial MCL (Medial Collateral Ligament) connects the medial epicondyle of the femur to the medial condyle of the tibia and resists valgus force
- Deep MCL (Medial Collateral Ligament) connects the medial epicondyle of the femur with the medial meniscus
- LCL (Lateral Collateral Ligament) entirely separate from the articular capsule, connects the lateral epicondyle of the femur to the head of the fibula and resists varus force
Knee Fracture
A fracture is a condition in which there is break in the continuity of the bone. In younger individuals these fractures are caused from high energy injuries, as from a motor vehicle accident. In older people the most common cause is weak and fragile bone.
Fractures of the knee can include the following:
Distal femur fracture: The distal femur is part of the femur bone that flares out like the mouth of the funnel. A distal femur (top part of knee joint) fracture is a break in thighbone that occurs just above your knee joint.
Femoral shaft fracture: A femoral shaft fracture is a break that occurs anywhere along the femoral shaft, long, straight part of the femur.
Fractures of proximal tibia: A proximal tibial fracture is a break in the upper part of the shin bone or tibia. Proximal tibial fractures may or may not involve the knee joint. Fractures that enter the knee joint may cause joint imperfections, irregular joint surfaces, and improper alignment in the legs. This can lead to as joint instability, arthritis, and loss of motion. These fractures are caused by stress or trauma or in a bone already compromised by disease, such as cancer or infection. Proximal tibia fractures can result in injury to the surrounding soft tissues including skin, muscle, nerves, blood vessels, and ligaments.
Tibial shaft fractures: A tibial shaft fracture is a break that occurs along the length of the tibia or shin bone (larger bone of the lower leg) between the knee and ankle joints. These fractures can occur while playing sports such as soccer
Diagnosis is made through your medical history, physical examination, and other diagnostic imaging tests. X-rays are taken to know whether the bone is intact or broken. X-rays are also helpful to know the type and location of fracture. Your doctor may also recommend a computerized tomography (CT) scan to know the severity of fracture.
Treatment options include non-surgical and surgical. Non-surgical treatment involves skeletal traction and use of casts and braces. Skeletal traction involves placement of pin into the bone in order to realign broken bones. Surgery involves internal fixation and external fixation.Internal Fixation
Intramedullary nailing: In this procedure a specially designed metal rod is placed into the marrow canal of the femur. Then the nail is passed on to reach the fracture site and keep it in place. The rod is secured in place with screws at both ends.
Plates and Screws fixation: In this procedure your surgeon will reposition the broken bone ends into normal position and then uses special screws or metal plates on the outer surface of the bone to hold the bone fragments in place.External Fixation
During the procedure, metal pins or screws are inserted into the middle of the femur and tibia and are attached to a device outside the skin to hold bone fragments in place to allow alignment and healing.
If your bone is fractured in many pieces, a plate or rod is fixed at both ends of the fracture to maintain the overall shape and length of the bone in place while it heals. In elder patients where fracture healing delays, a bone graft taken from the patient or tissue bank may be used to form callous. In severe case, the bone fragments are removed and the bone is replaced with a knee replacement implant.
The most common complications of surgery include infection, knee stiffness, delayed bone healing, and knee arthritis.Meniscus Tear
Meniscus tear is the commonest knee injury in athletes, especially those involved in contact sports. A suddenly bend or twist in your knee cause the meniscus to tear. This is a traumatic meniscus tear. Elderly people are more prone to degenerative meniscal tears as the cartilage wears out and weakens with age. The two wedge-shape cartilage pieces present between the thighbone and the shinbone are called meniscus. They stabilize the knee joint and act as “shock absorbers”.
Torn meniscus causes pain, swelling, stiffness, catching or locking sensation in your knee making you unable to move your knee through its complete range of motion. Your orthopedic surgeon will examine your knee, evaluate your symptoms, and medical history before suggesting a treatment plan. The treatment depends on the type, size and location of tear as well your age and activity level. If the tear is small with damage in only the outer edge of the meniscus, nonsurgical treatment may be sufficient. However, if the symptoms do not resolve with nonsurgical treatment, surgical treatment may be recommended.Surgical Treatment
Knee arthroscopy is the commonly recommended surgical procedure for meniscal tears. The surgical treatment options include meniscus removal (meniscectomy), meniscus repair, and meniscus replacement. Surgery can be performed using arthroscopy where a tiny camera will be inserted through a tiny incision which enables the surgeon to view inside of your knee on a large screen and through other tiny incisions, surgery will be performed. During meniscectomy, small instruments called shavers or scissors may be used to remove the torn meniscus. In arthroscopic meniscus repair the torn meniscus will be pinned or sutured depending on the extent of tear.
Meniscus replacement or transplantation involves replacement of a torn cartilage with the cartilage obtained from a donor or a cultured patch obtained from laboratory. It is considered as a treatment option to relieve knee pain in patients who have undergone meniscectomy.Mako Robotic-Arm Assisted Technology for Partial Knee Replacement
We understand that making sure you know what to expect from your joint replacement experience is important to you. As you are reading through this material, if you have additional questions please reach out to us to discuss.
Each patient is unique, and can experience joint pain for different reasons. It’s important to talk to us about the reason for your knee pain so you can understand the treatment options available to you. Pain from arthritis and joint degeneration can be constant or come and go, occur with movement or after a period of rest, or be located in one spot or many parts of the body. It is common for patients to try medication and other conservative treatments to treat their knee pain. If you haven’t experienced adequate relief with those treatment options, you may be a candidate for Mako Total Knee replacement, which may provide you with relief from your knee pain.How Mako Technology Works
Personalized Pre-operative Plan
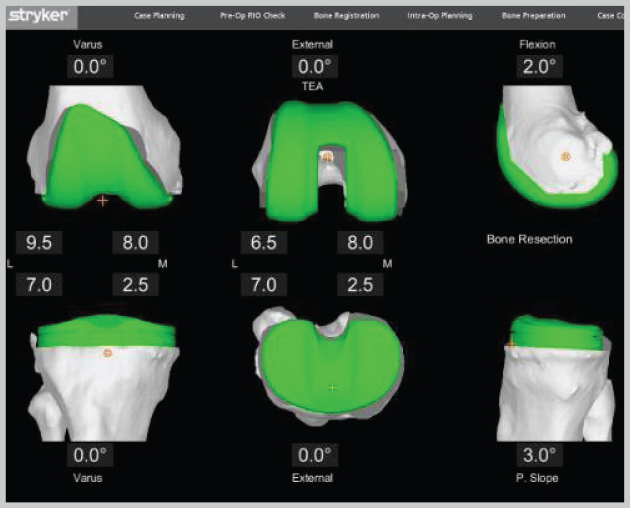
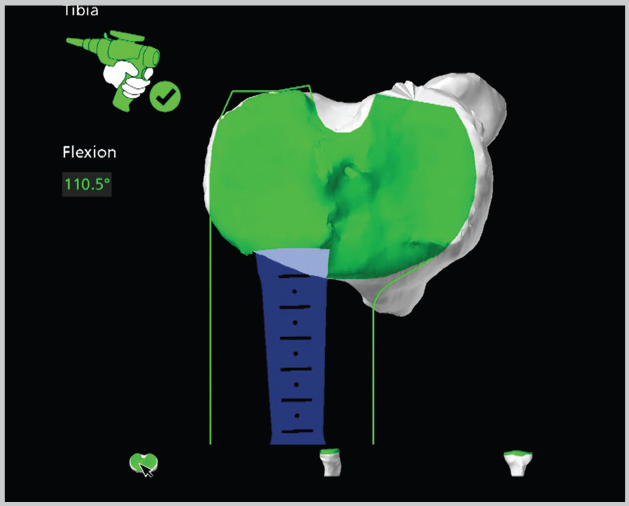
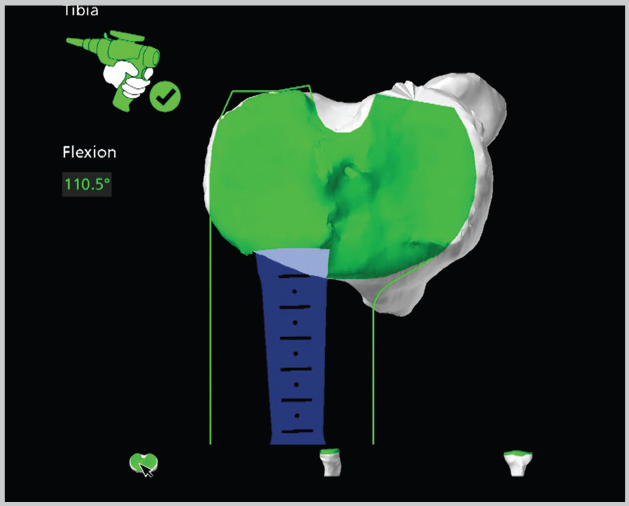
Bone Preparation
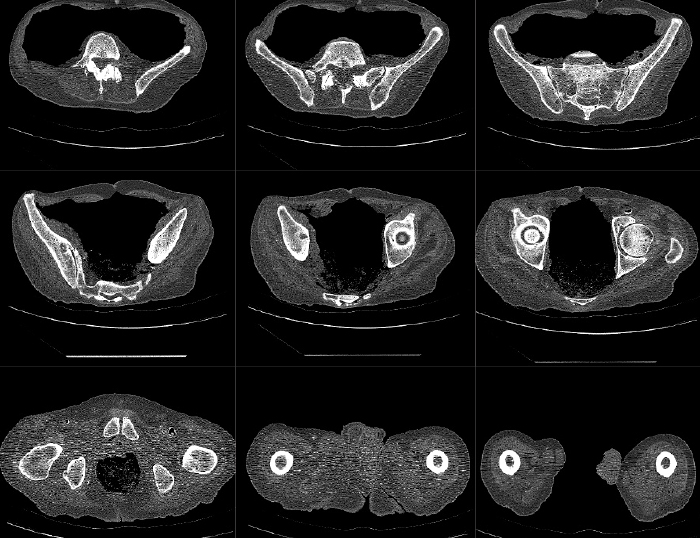
Mako Robotic-Arm Assisted Total Knee Replacement is a treatment option for adults living with mid to late-stage osteoarthritis (OA) of the knee. Mako provides you with a personalized surgical plan based on your unique anatomy. First, a CT scan of the diseased knee joint is taken. This CT scan is uploaded into the Mako System software, where a 3D model of your knee is created. This 3D model is used to pre-plan and assist your surgeon in performing your total knee replacement.
In the operating room, your surgeon follows your personalized surgical plan while preparing the bone for the Triathlon Total Knee implant. With over a decade of clinical history, Triathlon knee replacements are different than traditional knee replacements because they are designed to work with the body to promote natural-like circular motion.1-4
The surgeon guides the robotic-arm to remove diseased bone and cartilage within the pre-defined area and the Mako System helps the surgeon stay within the planned boundaries that were defined when the personalized pre-operative plan was created. In a laboratory study, Mako Technology demonstrated accurate placement of implants to a personalized surgical plan.5
It’s important to understand that the surgery is performed by an orthopedic surgeon, who guides the robotic-arm during the surgery to position the implant in the knee joint. The robotic-arm does not perform surgery, make decisions on its own, or move without the surgeon guiding the robotic-arm. The Mako System also allows your surgeon to make adjustments to your plan during surgery as needed.IMPORTANT INFORMATION
Knee Replacements
General indications: Total knee replacement is intended for use in individuals with joint disease resulting from degenerative, rheumatoid, and post-traumatic arthritis, and for moderate deformity of the knee.
Contraindications: Knee replacement surgery is not appropriate for patients with certain types of infections, any mental or neuromuscular disorder which would create an unacceptable risk of prosthesis instability, prosthesis fixation failure, or complications in postoperative care, compromised bone stock, skeletal immaturity, or severe instability of the knee.
As with any surgery, knee replacement surgery has serious risks which include, but are not limited to, peripheral neuropathies (nerve damage), circulatory compromise (including deep vein thrombosis (blood clots in the legs)), genitourinary disorders (including kidney failure), gastrointestinal disorders (including paralytic ileus (loss of intestinal digestive movement)), vascular disorders (including thrombus (blood clots), blood loss, or changes in blood pressure or heart rhythm), bronchopulmonary disorders (including emboli, stroke or pneumonia), heart attack, and death.
Implant related risks which may lead to a revision include dislocation, loosening, fracture, nerve damage, heterotopic bone formation (abnormal bone growth in tissue), wear of the implant, metal sensitivity, soft tissue imbalance, osteolysis (localized progressive bone loss), and reaction to particle debris. Knee implants may not provide the same feel or performance characteristics experienced with a normal healthy joint.
The information presented is for educational purposes only. Speak to your doctor to decide if joint replacement surgery is right for you. Individual results vary and not all patients will receive the same postoperative activity level. The lifetime of a joint replacement is not infinite and varies with each individual. Your doctor will help counsel you about how to best maintain your activities in order to potentially prolong the lifetime of the device. Such strategies include not engaging in high-impact activities, such as running, as well as maintaining a healthy weight. Ask your doctor if the Triathlon knee is right for you.
Stryker Corporation or its other divisions or other corporate affiliated entities own, use or have applied for the following trademarks or service marks: Mako, Stryker, Triathlon. All other trademarks are trademarks of their respected owners or holders.References
Mistry J, Elmallah R, Chughtai M, Oktem M, Harwin S, Mont M. Long-Term Survivorship and Clinical Outcomes of a Single Radius Total Knee Arthroplasty. International XXVIII.
Designed to maintain collateral ligament stability throughout the range of motion. Stryker-Initiated Dynamic Computer Simulations of Passive ROM and Oxford Rig Test, Stephen Piazza, 2003.
Wang H, Simpson KJ, Ferrara MS, Chamnongkich S, Kinsey T, Mahoney, OM. Biomechanical differences exhibited during sit-to-stand between total knee arthroplasty designs of varying radii. J Arthroplasty. 2006;21(8):1193-1199.
Gómez-Barrena E, Fernandez-García C, Fernandez- Bravo A, Cutillas-Ruiz R, Bermejo-Fernandez G. Functional performance with a single-radius femoral design total knee arthroplasty. Clin Ortho Relates Res. 2010;468(5):1214-1220.
Hampp E. et al. Robotic-Arm Assisted Total Knee Arthroplasty Demonstrated Greater Accuracy to Plan Compared to Manual Technique. Orthopaedic Research Society 2017 Annual Meeting, San Diego, CA. Poster No. 2412. March 20-22, 2017.
MKOHMT-PE-3_Rev-1_13841
Copyright © 2017 Stryker CorporationMako Robotic-Arm Assisted Technology for Total Knee Replacement
We understand that making sure you know what to expect from your joint replacement experience is important to you. As you are reading through this material, if you have additional questions please reach out to us to discuss.
Each patient is unique, and can experience joint pain for different reasons. It’s important to talk to us about the reason for your knee pain so you can understand the treatment options available to you. Pain from arthritis and joint degeneration can be constant or come and go, occur with movement or after a period of rest, or be located in one spot or many parts of the body. It is common for patients to try medication and other conservative treatments to treat their knee pain. If you haven’t experienced adequate relief with those treatment options, you may be a candidate for Mako Total Knee replacement, which may provide you with relief from your knee pain.How Mako Technology Works
Personalized Pre-operative Plan
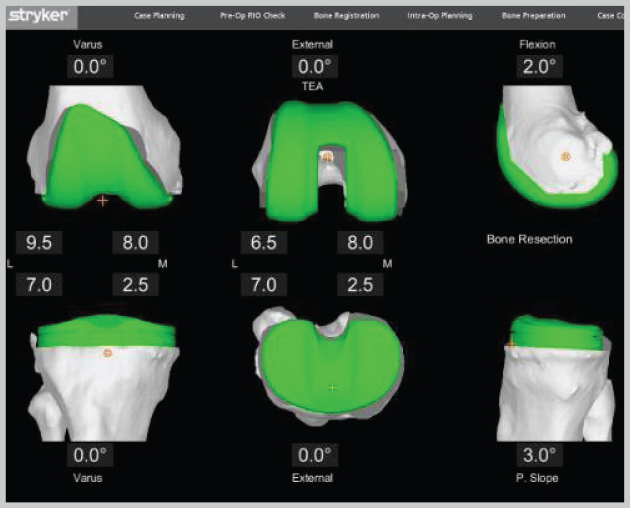
Bone Preparation
Mako Robotic-Arm Assisted Total Knee Replacement is a treatment option for adults living with mid to late-stage osteoarthritis (OA) of the knee. Mako provides you with a personalized surgical plan based on your unique anatomy. First, a CT scan of the diseased knee joint is taken. This CT scan is uploaded into the Mako System software, where a 3D model of your knee is created. This 3D model is used to pre-plan and assist your surgeon in performing your total knee replacement.
In the operating room, your surgeon follows your personalized surgical plan while preparing the bone for the Triathlon Total Knee implant. With over a decade of clinical history, Triathlon knee replacements are different than traditional knee replacements because they are designed to work with the body to promote natural-like circular motion.1-4
The surgeon guides the robotic-arm to remove diseased bone and cartilage within the pre-defined area and the Mako System helps the surgeon stay within the planned boundaries that were defined when the personalized pre-operative plan was created. In a laboratory study, Mako Technology demonstrated accurate placement of implants to a personalized surgical plan.5
It’s important to understand that the surgery is performed by an orthopedic surgeon, who guides the robotic-arm during the surgery to position the implant in the knee joint. The robotic-arm does not perform surgery, make decisions on its own, or move without the surgeon guiding the robotic-arm. The Mako System also allows your surgeon to make adjustments to your plan during surgery as needed.IMPORTANT INFORMATION
Knee Replacements
General indications: Total knee replacement is intended for use in individuals with joint disease resulting from degenerative, rheumatoid, and post-traumatic arthritis, and for moderate deformity of the knee.
Contraindications: Knee replacement surgery is not appropriate for patients with certain types of infections, any mental or neuromuscular disorder which would create an unacceptable risk of prosthesis instability, prosthesis fixation failure, or complications in postoperative care, compromised bone stock, skeletal immaturity, or severe instability of the knee.
As with any surgery, knee replacement surgery has serious risks which include, but are not limited to, peripheral neuropathies (nerve damage), circulatory compromise (including deep vein thrombosis (blood clots in the legs)), genitourinary disorders (including kidney failure), gastrointestinal disorders (including paralytic ileus (loss of intestinal digestive movement)), vascular disorders (including thrombus (blood clots), blood loss, or changes in blood pressure or heart rhythm), bronchopulmonary disorders (including emboli, stroke or pneumonia), heart attack, and death.
Implant related risks which may lead to a revision include dislocation, loosening, fracture, nerve damage, heterotopic bone formation (abnormal bone growth in tissue), wear of the implant, metal sensitivity, soft tissue imbalance, osteolysis (localized progressive bone loss), and reaction to particle debris. Knee implants may not provide the same feel or performance characteristics experienced with a normal healthy joint.
The information presented is for educational purposes only. Speak to your doctor to decide if joint replacement surgery is right for you. Individual results vary and not all patients will receive the same postoperative activity level. The lifetime of a joint replacement is not infinite and varies with each individual. Your doctor will help counsel you about how to best maintain your activities in order to potentially prolong the lifetime of the device. Such strategies include not engaging in high-impact activities, such as running, as well as maintaining a healthy weight. Ask your doctor if the Triathlon knee is right for you.
Stryker Corporation or its other divisions or other corporate affiliated entities own, use or have applied for the following trademarks or service marks: Mako, Stryker, Triathlon. All other trademarks are trademarks of their respected owners or holders.References
Mistry J, Elmallah R, Chughtai M, Oktem M, Harwin S, Mont M. Long-Term Survivorship and Clinical Outcomes of a Single Radius Total Knee Arthroplasty. International XXVIII.
Designed to maintain collateral ligament stability throughout the range of motion. Stryker-Initiated Dynamic Computer Simulations of Passive ROM and Oxford Rig Test, Stephen Piazza, 2003.
Wang H, Simpson KJ, Ferrara MS, Chamnongkich S, Kinsey T, Mahoney, OM. Biomechanical differences exhibited during sit-to-stand between total knee arthroplasty designs of varying radii. J Arthroplasty. 2006;21(8):1193-1199.
Gómez-Barrena E, Fernandez-García C, Fernandez- Bravo A, Cutillas-Ruiz R, Bermejo-Fernandez G. Functional performance with a single-radius femoral design total knee arthroplasty. Clin Ortho Relates Res. 2010;468(5):1214-1220.
Hampp E. et al. Robotic-Arm Assisted Total Knee Arthroplasty Demonstrated Greater Accuracy to Plan Compared to Manual Technique. Orthopaedic Research Society 2017 Annual Meeting, San Diego, CA. Poster No. 2412. March 20-22, 2017.
MKOHMT-PE-3_Rev-1_13841
Copyright © 2017 Stryker CorporationPatellofemoral Instability
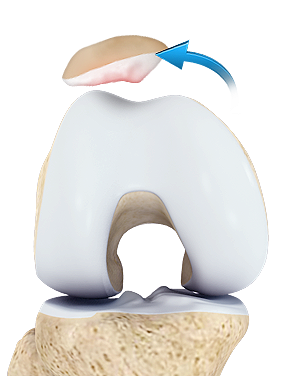
The knee can be divided into three compartments: patellofemoral, medial and lateral compartment. The patellofemoral compartment is the compartment in the front of the knee between the knee cap and thigh bone. The medial compartment is the area on the inside portion of the knee, and the lateral compartment is the area on the outside portion of the knee joint. Patellofemoral instability means that the patella (kneecap) moves out of its normal pattern of alignment. This malalignment can damage the underlying soft structures such as muscles and ligaments that hold the knee in place.
Causes
Patellofemoral instability can be caused because of variations in the shape of the patella or its trochlear groove as the knee bends and straightens. Normally, the patella moves up and down within the trochlear groove when the knee is bent or straightened. Patellofemoral instability occurs when the patella moves either partially (subluxation) or completely (dislocation) out of the trochlear groove.
A combination of factors can cause this abnormal tracking and include the following:
Anatomical defect - Flat feet or fallen arches and congenital abnormalities in the shape of the patella bone can cause misalignment of the knee joint.
Abnormal Q angle - The high Q angle (angle between the hips and knees) often results in mal tracking of the patella such as in patients with knock knees.
Patellofemoral arthritis - Patellofemoral arthritis occurs when there is a loss of the articular cartilage on the back of the kneecap. This can eventually lead to abnormal tracking of the patella.
Improper muscle balance - Weak quadriceps (anterior thigh muscles) can lead to abnormal tracking of the patella, causing it subluxate or dislocate.
Young active individuals involved in sports activities are more prone to patellofemoral instability.Symptoms
Patellofemoral instability causes pain when standing up from a sitting position and a feeling that the knee may buckle or give way. When the kneecap slips partially or completely you may have severe pain, swelling, bruising, visible deformity and loss of function of the knee. You may also have sensational changes such as numbness or even partial paralysis below the dislocation as a result of pressure on nerves and blood vessels.
Diagnosis
Your doctor evaluates the source of patellofemoral instability based on your medical history and physical examination. Other diagnostic tests such as X-rays, MRI and CT scan may be done to determine the cause of your knee pain and to rule out other conditions.
Conservative treatment
If your kneecap is only partially dislocated (subluxation), your physician may recommend non-surgical treatments, such as pain medications, rest, ice, physical therapy, knee-bracing, and orthotics. If the kneecap has been completely dislocated, the kneecap may need to be repositioned back in its proper place in the groove. This process is called closed reduction.
Surgical treatment
Surgery is sometimes needed to help return the patella to a normal tracking path when other non-surgical treatments have failed. The aim of the surgery is to realign the kneecap in the groove and to decrease the Q angle. Patellar realignment surgery is broadly classified into proximal re-alignment procedures and distal re-alignment procedures. Proximal re-alignment procedures: During this procedure, structures that limit the movements on the outside of the patella are lengthened or ligaments on the inside of the patella are shortened. Distal re-alignment procedures: During this procedure, the Q angle is decreased by moving the tibial tubercle towards the inner side of the knee. The surgery is performed under sterile conditions in the operating room under spinal or general anesthesia. The surgeon will make two or three small cuts around your knee. The arthroscope, a narrow tube with a tiny camera on the end is inserted through one of the incisions to view the knee joint. Specialized instruments are inserted into the joint through other small incisions. The camera attached to the arthroscope displays the image of the joint on the monitor. A sterile solution will be pumped into your knee in order to stretch the knee and provide a clear view and room for the surgeon to work. With the images from the arthroscope as a guide the surgeon can look for any pathology or anomaly and repair it through the other incisions with various instruments. After the evaluation is completed, a larger incision is made over the front of the knee. Depending on your situation, a lateral retinacular release may be performed. In this procedure, the tight ligaments on the outer side of the knee are released, thus allowing the patella to sit properly in the femoral groove. Your surgeon may also tighten the tendons on the inside, or medial side of the knee to realign the quadriceps. In cases where the malalignment is severe, a procedure called a tibial tubercle transfer (TTT) will be performed. In this procedure a section of bone where the patellar tendon attaches to the tibia is removed. This bony section is then shifted and properly realigned with the patella and reattached to the tibia using screws. Once the malalignment is repaired and confirmed with arthroscopic evaluation, the incisions are closed with sutures.
Postoperative care
Your doctor will recommend pain medications to relieve pain. To help reduce the swelling you will be instructed to elevate the leg and apply ice packs over the knee. Crutches are necessary for the first few weeks to prevent weight bearing on the knee. A knee immobilizer may be used to stabilize the knee. You will be instructed about the activities to be avoided and exercises to be performed for a faster recovery. A rehabilitation program may be advised for a speedy recovery.
Risks and complications
Possible risks and complications associated with the surgery include:
- Loss of ability to extend the knee
- Recurrent dislocations or subluxations
- Arthrofibrosis (thick fibrous material around the joint)
- Persistent pain
Patients with patellofemoral instability have problems with the alignment of the knee cap. Therefore, treatment is necessary to bring the knee cap back into normal alignment. Your surgeon will decide which procedure is appropriate for your particular situation.
Knee Osteoarthritis
Osteoarthritis, also called degenerative joint disease is the most common form of arthritis. It occurs most often in older people. This disease affects the tissue covering the ends of bones in a joint (cartilage). In a person with osteoarthritis, the cartilage becomes damaged and worn out causing pain, swelling, stiffness and restricted movement in the affected joint. This condition most commonly affects the joints in hips, knees, hands, and spine. Rarely, the disease may affect the shoulders, wrists and feet.
Causes and risk factors
Osteoarthritis is caused by the wearing out of the cartilage covering the bone ends in a joint. This may be due to being overweight, excessive strain over prolonged periods of time, previous fracture, growth abnormalities, joint diseases, injury or deformity.
Some people have congenital abnormalities of the joints that cause early degeneration and subsequently cause osteoarthritis.Diagnosis
Doctors diagnose osteoarthritis with a medical history, physical exam and x-rays of the affected joint. During the physical examination, your doctor will examine the affected joint for swelling, pain, tenderness, and assess the joint’s range of motion. An X-ray of the knee may show a loss of the joint space and bone spur formation.
There is no blood test for osteoarthritis.Treatment
There is no known cure for osteoarthritis; however, there are several treatments and lifestyle modifications that can help you ease your pain and symptoms. The objective of the treatment is to reduce pain, improve joint movement, and prevent further damage to joint. The treatment of osteoarthritis involves:
- Medications: Medications may include different classes such as anti-inflammatory drugs, steroid injections, artificial joint fluid injections, and other drugs.
Lifestyle Modifications
Some of the lifestyle modifications include:
- A moderate exercise program
- Use of Heat or cold treatments
- Eating a healthy and well balanced diet
- Get adequate rest
- Lose weight
- Protect your joints with the use of assistive devices such as splints or braces to support the weakened joints
- Physical therapy: Your physical therapist will teach you exercises to keep joints flexible and improve muscle strength.
- Surgery: Surgery is usually considered if nonsurgical treatment fails to provide relief. Joint replacement surgery is considered as an option when the pain is so severe that it affects your ability to carry out normal activities.
Total Knee Replacement (TKR)

Total knee replacement, also called total knee arthroplasty, is a surgical procedure in which the worn out or damaged surfaces of the knee joint are removed and replaced with artificial parts. The knee is made up of the femur (thigh bone), the tibia (shin bone), and patella (kneecap). The meniscus, the soft cartilage between the femur and tibia, serves as a cushion and helps absorb shock during motion. Arthritis (inflammation of the joints), injury, or other diseases of the joint can damage this protective layer of cartilage, causing extreme pain and difficulty in performing daily activities. Your doctor may recommend surgery if non-surgical treatment options have failed to relieve the symptoms.
Indications
Total knee replacement surgery is commonly indicated for severe osteoarthritis of the knee. Osteoarthritis is the most common form of knee arthritis in which the joint cartilage gradually wears away. It often affects older people.
In a normal joint, articular cartilage allows for smooth movement within the joint, whereas in an arthritic knee the cartilage itself becomes thinner or completely absent. In addition, the bones become thicker around the edges of the joint and may form bony “spurs”. All of these factors can cause pain and restricted range of motion in the joint.Your doctor may advise total knee replacement if you have:
- Severe knee pain which limits your daily activities (such as walking, getting up from a chair or climbing stairs).
- Moderate to severe pain that occurs during rest or awakens you at night.
- Chronic knee inflammation and swelling that is not relieved with rest or medications.
- Failure to obtain pain relief from medications, injections, physical therapy, or other conservative treatments.
- A bow- legged knee deformity.
Causes
The exact cause of osteoarthritis is not known, however there are a number of factors that are commonly associated with the onset of arthritis and may include:
- Injury or trauma to the joint
- Fractures at the knee joint
- Increased body weight
- Repetitive overuse
- Joint infection
- Inflammation of the joint
- Connective tissue disorders
Diagnosis
Your doctor will diagnose osteoarthritis based on the medical history, physical examination, and X-rays.
X-rays typically show a narrowing of the joint space in the arthritic knee.
Procedure
The goal of total knee replacement surgery is to relieve pain and restore the alignment and function of your knee.
The surgery is performed under spinal or general anesthesia. Your surgeon will make an incision in the skin over the affected knee to expose the knee joint. Then the damaged portions of the femur bone are cut at appropriate angles using specialized jigs. The femoral component is attached to the end of the femur with or without bone cement. The surgeon then cuts or shaves the damaged area of the tibia (shinbone) and the cartilage. This removes the deformed part of the bone and any bony growths, as well as creates a smooth surface on which the implants can be attached. Next, the tibial component is secured to the end of the bone with bone cement or screws. Your surgeon will place a plastic piece called an articular surface between the implants to provide a smooth gliding surface for movement. This plastic insert will support the body’s weight and allow the femur to move over the tibia, similar to the original meniscus cartilage. The femur and the tibia with the new components are then put together to form the new knee joint. To make sure the patella (knee cap) glides smoothly over the new artificial knee, its rear surface is also prepared to receive a plastic component. With all the new components in place, the knee joint is tested through its range of motion. The entire joint is then irrigated and cleaned with a sterile solution. The incision is carefully closed, drains are inserted and a sterile dressing is placed over the incision.Post-operative care
Rehabilitation begins immediately following the surgery. A physical therapist will teach you specific exercises to strengthen your leg and restore knee movement. Knee immobilizers are used to stabilize the knee. You will be able to walk with crutches or a walker. A continuous passive motion (CPM) machine can be used to move the knee joint . Continuous passive motion is a device attached to the treated leg which constantly moves the joint through a controlled range of motion, while the patient relaxes. Your physical therapist will also provide you with a home exercise program to strengthen thigh and calf muscles.
Risks and complications
As with any major surgery, possible risks and complications associated with total knee replacement surgery include:
- Knee stiffness
- Infection
- Blood clots (deep vein thrombosis)
- Nerve and blood vessel damage
- Ligament injuries
- Patella (kneecap) dislocation
- Plastic liner wears out
- Loosening of the implant
If you find difficulty in performing simple activities such as walking or climbing stairs because of your severe arthritic knee pain, then total knee replacement may be an option for you. It is a safe and effective procedure to relieve pain, correct leg deformity, and help you resume your normal activities of daily living.
Bilateral Replacement
For those patients that have two painful arthritic knees replacing both at the same time may be the best option. When both knees require reconstructive surgery to overcome painful unsteady ambulation, your surgeon may recommend simultaneous bilateral knee replacement. That is having both knees replaced at the same time under one anesthetic and one stent of physical therapy to rehabilitate full function in both knees at the same time. It is not twice the pain but it is half the time to full recovery.
Over the last 15 years Dr Sikes and Dr Stonnington have refined the process by working together to lead two surgical teams in an orchestrated process of precision surgery such that both total knee replacements are completed in a rapid manner. Our skilled therapist will coach this specially selected patient group to begin walking with a walker within hours after surgery.
The refined pathways of care including careful pre-op medical review, two surgeon cooperation, rapid surgical time, and multimodal pain management have made this group a particularly satisfying success story. The amazingly successful results for these double knee replacement patients is a documented quality outcome that contradicts some poor outcomes reported in the orthopedic literature of decades’ past.
To consider having both knees replaced may be an opportunity at a total victory rather than just solving half the problem and being forced to complete the process again.Ligament Reconstruction
Anterior Cruciate Ligament ACL Reconstruction
The anterior cruciate ligament is one of the major stabilizing ligaments in the knee. It is a strong rope like structure located in the center of the knee running from the femur to the tibia. When this ligament tears unfortunately, it does not heal and often leads to the feeling of instability in the knee.
ACL reconstruction is a commonly performed surgical procedure and with recent advances in arthroscopic surgery can now be performed with minimal incision and low complication rates.ACL Reconstruction Hamstring Tendon
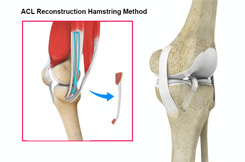
Anterior cruciate ligament (ACL) reconstruction hamstring method is a surgical procedure that replaces the injured ACL with a hamstring tendon. Anterior cruciate ligament is one of the four major ligaments of the knee that connects the femur (thigh bone) to the tibia (shin bone) and helps stabilize your knee joint. Anterior cruciate ligament prevents excessive forward movement of the lower leg bone (the tibia) in relation to the thigh bone (the femur) as well as limits rotational movements of the knee.
A tear of this ligament can make you feel as though your knees will not allow you to move or even hold you up. Anterior cruciate ligament reconstruction is surgery to reconstruct the torn ligament of your knee with a tissue graft.Causes
An ACL injury most commonly occurs during sports that involve twisting or overextending your knee. An ACL can be injured in several ways:
- Sudden directional change
- Slowing down while running
- Landing from a jump incorrectly
- Direct blow to the side of your knee, such as during a football tackle
Symptoms
When you injure your ACL, you might hear a loud “pop” sound and you may feel the knee buckle. Within a few hours after an ACL injury, your knee may swell due to bleeding from vessels within the torn ligament. You may notice that the knee feels unstable or seems to give way, especially when trying to change direction on the knee.
Diagnosis
An ACL injury can be diagnosed with a thorough physical examination of the knee and diagnostic tests such as X-rays, MRI scans and arthroscopy. X-rays may be needed to rule out any fractures. In addition, your doctor will often perform the Lachman’s test to see if the ACL is intact. During a Lachman test, knees with a torn ACL may show increased forward movement of the tibia and a soft or mushy endpoint compared to a healthy knee.
Pivot shift test is another test to assess ACL tear. During this test, if the ACL is torn, the tibia will move forward when the knee is completely straight and as the knee bends past 30° the tibia shifts back into correct place in relation to the femur.Procedure
The goal of ACL reconstruction surgery is to tighten your knee and to restore its stability.
Anterior cruciate ligament reconstruction hamstring method is a surgical procedure to replace the torn ACL with part of the hamstring tendon taken from the patient’s leg. The Hamstring is the muscle located on the back of your thigh. The procedure is performed under general anesthesia. Your surgeon will make two small cuts about 1/4 inch long around your knee. An arthroscope, a tube with a small video camera on the end is inserted through one incision to see the inside of the knee joint. Along with the arthroscope, a sterile solution is pumped into the joint to expand it enabling the surgeon to have a clear view and space to work inside the joint. The knee is bent at right angles and the hamstring tendons felt. A small incision is made over the hamstring tendon attachment to the tibia and the two tendons are stripped off the muscle and the graft is prepared. The torn ACL will be removed and the pathway for the new ACL is prepared. The arthroscope is reinserted into the knee joint through one of the small incisions. Small holes are drilled into the upper and lower leg bones where these bones come together at the knee joint. The holes form tunnels in your bone to accept the new graft. Then the graft is pulled through the predrilled holes in the tibia and femur. The new tendon is then fixed into the bone with screws to hold it into place while the ligament heals into the bone. The incisions are then closed with sutures and a dressing is placed.Risks and Complications
Possible risks and complications associated with ACL reconstruction with hamstring method include:
- Numbness
- Infection
- Blood clots(Deep vein thrombosis)
- Nerve and blood vessel damage
- Failure of the graft
- Loosening of the graft
- Decreased range of motion
- Crepitus (crackling or grating feeling of the kneecap)
- Pain in the knee
- Repeat injury to the graft
Post-Operative Care
Following the surgery, rehabilitation begins immediately. A physical therapist will teach you specific exercises to be performed to strengthen your leg and restore knee movement. Avoid competitive sports for 5 to 6 months to allow the new graft to incorporate into the knee joint.
Anterior cruciate ligament reconstruction is a very common and successful procedure. It is usually indicated in patients wishing to return to an active lifestyle especially those wishing to play sports involving running and twisting. Anterior cruciate ligament injury is a common knee ligament injury. If you have injured your ACL, surgery may be needed to regain full function of your knee.ACL Reconstruction Patellar Tendon
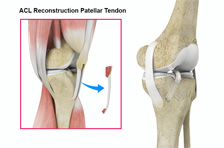
Anterior cruciate ligament (ACL) reconstruction patellar tendon is a surgical procedure that replaces the injured ACL with a patellar tendon. Anterior cruciate ligament is one of the four major ligaments of the knee that connects the femur (thigh bone) to the tibia (shin bone) and helps stabilize the knee joint. Anterior cruciate ligament prevents excessive forward movement of the lower leg bone (tibia) in relation to the thigh bone (femur) as well as limits rotational movements of the knee.
A tear of this ligament can make you feel as though your knees will not allow you to move or even hold you up. Anterior cruciate ligament reconstruction is surgery to reconstruct the torn ligament of your knee with a tissue graft.Causes
An ACL injury most commonly occurs during sports that involve twisting or overextending your knee. The ACL can be injured in several ways:
- Sudden directional change
- Slowing down while running
- Landing from a jump incorrectly
- Direct blow to the side of your knee, such as during a football tackle
Symptoms
When you injure your ACL, you might hear a loud “pop” sound and you may feel the knee buckle. Within a few hours after an ACL injury, your knee may swell due to bleeding from vessels within the torn ligament. You may notice that the knee feels unstable or seems to give way, especially when trying to change direction on the knee.
Diagnosis
An ACL injury can be diagnosed with a thorough physical examination of the knee and diagnostic tests such as X-rays, MRI scans and arthroscopy. X-rays may be needed to rule out any fractures.
In addition, your doctor will often perform the Lachman’s test to see if the ACL is intact. During a Lachman test, knees with a torn ACL may show increased forward movement of the tibia and a soft or mushy endpoint compared to a healthy knee.
Pivot shift test is another test to assess ACL tear. During the pivot shift test, if the ACL is torn the tibia will move forward when the knee is completely straight and as the knee bends past 30° the tibia shifts back into correct place in relation to the femur.Procedure
The goal of ACL reconstruction surgery is to tighten your knee and to restore its stability.
Anterior cruciate ligament reconstruction patellar tendon is a surgical procedure to replace the torn ACL with part of the patellar tendon taken from the patient’s leg. The new ACL is harvested from the patellar tendon that connects the bottom of the kneecap (patella) to the top of the shinbone (tibia).The procedure is performed under general anesthesia. Your surgeon will make two small cuts about ¼ inch around your knee. An arthroscope, a tube with a small video camera on the end is inserted through one incision to see the inside of the knee joint. Along with the arthroscope, a sterile solution is pumped into the knee to expand it providing the surgeon a clear view of the inside of the joint. The torn ACL will be removed and the pathway for the new ACL is prepared. Your surgeon makes an incision over the patellar tendon and takes out the middle third of the patellar tendon, along with small plugs of bone where it is attached on each end. The remaining portions of the patellar tendon on either side of the graft are sutured back after its removal. Then the incision is closed. The arthroscope is reinserted into the knee joint through one of the small incisions. Small holes are drilled into the upper and lower leg bones where these bones come together at the knee joint. The holes form tunnels in your bone to accept the new graft. Then the graft is pulled through the predrilled holes in the tibia and femur. The new tendon is then fixed into the bone with screws to hold it into place while the ligament heals into the bone. The incisions are then closed with sutures and a dressing is placed.Risks and complications
Possible risks and complications associated with ACL reconstruction with patellar tendon method include:
- Numbness
- Infection
- Blood clots (Deep vein thrombosis)
- Nerve and blood vessel damage
- Failure of the graft
- Loosening of the graft
- Decreased range of motion
- Crepitus (crackling or grating feeling of the kneecap)
- Pain in the knee
- Repeat injury to the graft
Post-operative care
Following the surgery rehabilitation begins immediately. A physical therapist will teach you specific exercises to strengthen your leg and restore knee movement. Avoid competitive sports for 5 to 6 months to allow the new graft to incorporate into the knee joint.
Anterior cruciate ligament reconstruction is a very common and successful procedure. It is usually indicated in patients who desire to return to an active lifestyle especially those wishing to play sports involving running and twisting. Anterior cruciate ligament injury is a common knee ligament injury. If you have injured your anterior cruciate ligament, surgery may be needed to regain full function of your knee. -
Hip
- Normal Anatomy of the Hip Joint
- Femoro Acetabular Impingement (FAI)
- Hip Fracture
- Mako Robotic-Arm Assisted Technology for Total Hip Replacement
- Total Hip Replacement (THR)
- Computer Navigated Surgery
- Direct Anterior Hip Replacement
Normal Anatomy of the Hip Joint
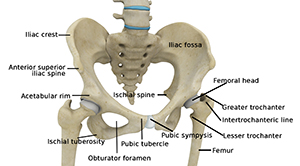
The thigh bone, femur, and the pelvis, acetabulum, join to form the hip joint. The hip joint is a “ball and socket” joint. The “ball” is the head of the femur, or thigh bone, and the “socket” is the cup shaped acetabulum.
The joint surface is covered by a smooth articular surface that allows pain free movement in the joint.
The cartilage cushions the joint and allows the bones to move on each other with smooth movements. This cartilage does not show up on X-ray, therefore you can see a “joint space” between the femoral head and acetabular socket.Pelvis
The pelvis is a large, flattened, irregularly shaped bone, constricted in the center and expanded above and below. It consists of three parts: the ilium, ischium, and pubis.
The socket, acetabulum, is situated on the outer surface of the bone and joins to the head of the femur to form the hip joint.Femur
The femur is the longest bone in the skeleton. It joins to the pelvis, acetabulum, to form the hip joint.
Femoro Acetabular Impingement (FAI)
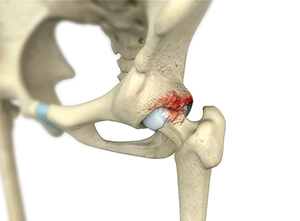
Femoroacetabular impingement (FAI) is a condition where there is too much friction in the hip joint from bony irregularities causing pain and decreased range of hip motion. The femoral head and acetabulum rub against each other creating damage and pain to the hip joint. The damage can occur to the articular cartilage (the smooth white surface of the ball or socket) or the labral tissue (the lining of the edge of the socket) during normal movement of the hip. The articular cartilage or labral tissue can fray or tear after repeated friction. Over time, more cartilage and labrum is lost until eventually the femur bone and acetabulum bone impact on one other. Bone on bone friction is commonly referred to as Osteoarthritis.
FAI impingement generally occurs as two forms: Cam and Pincer.
CAM Impingement: The Cam form of impingement is when the femoral head and neck are not perfectly round, most commonly due to excess bone that has formed. This lack of roundness and excess bone causes abnormal contact between the surfaces.
PINCER Impingement: The Pincer form of impingement is when the socket or acetabulum rim has overgrown and is too deep. It covers too much of the femoral head resulting in the labral cartilage being pinched. The Pincer form of impingement may also be caused when the hip socket is abnormally angled backwards causing abnormal impact between the femoral head and the rim of the acetabulum.
Most diagnoses of FAI include a combination of the Cam and Pincer forms.Symptoms of FAI
Symptoms of femoroacetabular impingement can include the following:
- Groin pain associated with hip activity
- Complaints of pain in the front, side or back of the hip
- Pain may be described as a dull ache or sharp pain
- Patients may complain of a locking, clicking, or catching sensation in the hip
- Pain often occurs to the inner hip or groin area after prolonged sitting or walking
- Difficulty walking uphill
- Restricted hip movement
- Low back pain
- Pain in the buttocks or outer thigh area
Risk Factors
A risk factor is something that is likely to increase a person’s chance of developing a disease or condition. Risk factors for developing femoroacetabular impingement may include the following:
- Groin pain associated with hip activity
- Complaints of pain in the front, side or back of the hip
- Pain may be described as a dull ache or sharp pain
- Patients may complain of a locking, clicking, or catching sensation in the hip
- Pain often occurs to the inner hip or groin area after prolonged sitting or walking
- Difficulty walking uphill
- Restricted hip movement
- Low back pain
- Pain in the buttocks or outer thigh area
Diagnosis
- Hip conditions should be evaluated by an orthopedic hip surgeon for proper diagnosis and treatment.
- Medical History
- Physical Examination
- Diagnostic studies including X-rays, MRI scans and CT Scan
Treatment Options
Conservative treatment options refer to management of the problem without surgery. Nonsurgical management of FAI will probably not change the underlying abnormal biomechanics of the hip causing the FAI but may offer pain relief and improved mobility.
Conservative treatment measures- Rest
- Activity Modification and Limitations
- Anti-inflammatory Medications
- Physical Therapy
- Injection of steroid and analgesic into the hip joint
Surgical treatment
Hip arthroscopy to repair femoroacetabular impingement is indicated when conservative treatment measures fail to provide relief to the patient.
Hip Fracture

The hip joint is a “ball and socket” joint. The “ball” is the head of the femur, or thigh bone, and the “socket” is the cup shaped acetabulum. The joint surface is covered by a smooth articular surface that allows pain free movement in the joint.
Hip fracture is a break that occurs near the hip in the upper part of the femur or thigh bone. The thigh bone has two bony processes on the upper part - the greater and lesser trochanters. The lesser trochanter projects from the base of the femoral neck on the back of the thigh bone. Hip fractures can occur either due to a break in the femoral neck, in the area between the greater and lesser trochanter or below the lesser trochanter.
Hip fracture is most frequently caused after minor trauma in elderly patients with weak bones, and by a high-energy trauma or serious injuries in young people. Long term use of certain medicines, such as bisphosphonates to treat osteoporosis (a disease causing weak bones) and other bone diseases, increases the risk of hip fractures.Signs and Symptoms
Signs and symptoms of hip fracture include:
- Pain in the groin or outer upper thigh
- Swelling and tenderness
- Discomfort while rotating the hip
- Shortening of the injured leg
- Outward or inward turning of the foot and knee of the injured leg
Your doctor may order an X-ray to diagnose your hip fracture. Other imaging tests, such as the magnetic resonance imaging or (MRI), may also be performed to detect the fracture.
Depending on the area of the upper femur involved, hip fractures are classified as- Intracapsular Fracture
- Intertrochanteric Fracture
- Subtrochanteric Fracture
Hip fractures can be corrected and aligned with non-operative and operative methods:
Traction may be an option to treat your condition if you are not fit for surgery. Skeletal traction may be applied under local anesthesia, where screws, pins and wires inserted into the femur, and a pulley system is set up at the end of the bed to bear heavy weights. These heavy weights help in correcting the misaligned bones until the injury heals.
Hip fractures can be surgically treated with external fixation, intramedullary fixation, or by using plates and screws.Mako Robotic-Arm Assisted Technology for Total Hip Replacement
We understand that making sure you know what to expect from the joint replacement experience is important to you. As you are reading through this material, if you have additional questions please reach out to us to discuss.
Each patient is unique, and can experience joint pain for different reasons. It’s important to talk to us about the reason for your hip pain so you can understand the treatment options available to you. Pain from arthritis and joint degeneration can be constant or come and go, occur with movement or after a period of rest, or be located in one spot or many parts of the body. It is common for patients to try medication and other conservative treatments to treat their hip pain. If you haven’t experienced adequate relief with those treatment options, you may be a candidate for Mako Total Hip replacement, which may provide you with relief from your hip pain.
Mako Robotic-Arm Assisted Technology provides you with a personalized surgical plan based on your unique anatomy. First, a CT scan of the diseased joint is taken. This CT scan is uploaded into the Mako System software, where a 3D model of your hip is created. This 3D model is used to pre-plan and assist your surgeon in performing your total hip replacement.
In the operating room, your surgeon follows your personalized surgical plan while preparing the bone for the implant. The surgeon guides the robotic-arm within the pre-defined area and the Mako System. The surgeon guides the robotic-arm within the pre-defined area and the Mako System helps the surgeon stay within the planned boundaries that were defined when the personalized pre-operative plan was created. This helps to provide more accurate placement and alignment of your implant. 1,2
Mako Robotic-Arm Assisted Total Hip replacement is a surgical procedure intended for patients who suffer from non-inflammatory or inflammatory degenerative joint disease (DJD). Some forms of DJD include osteoarthritis (OA), post-traumatic arthritis, rheumatoid arthritis (RA), avascular necrosis (AVN) and hip dysplasia.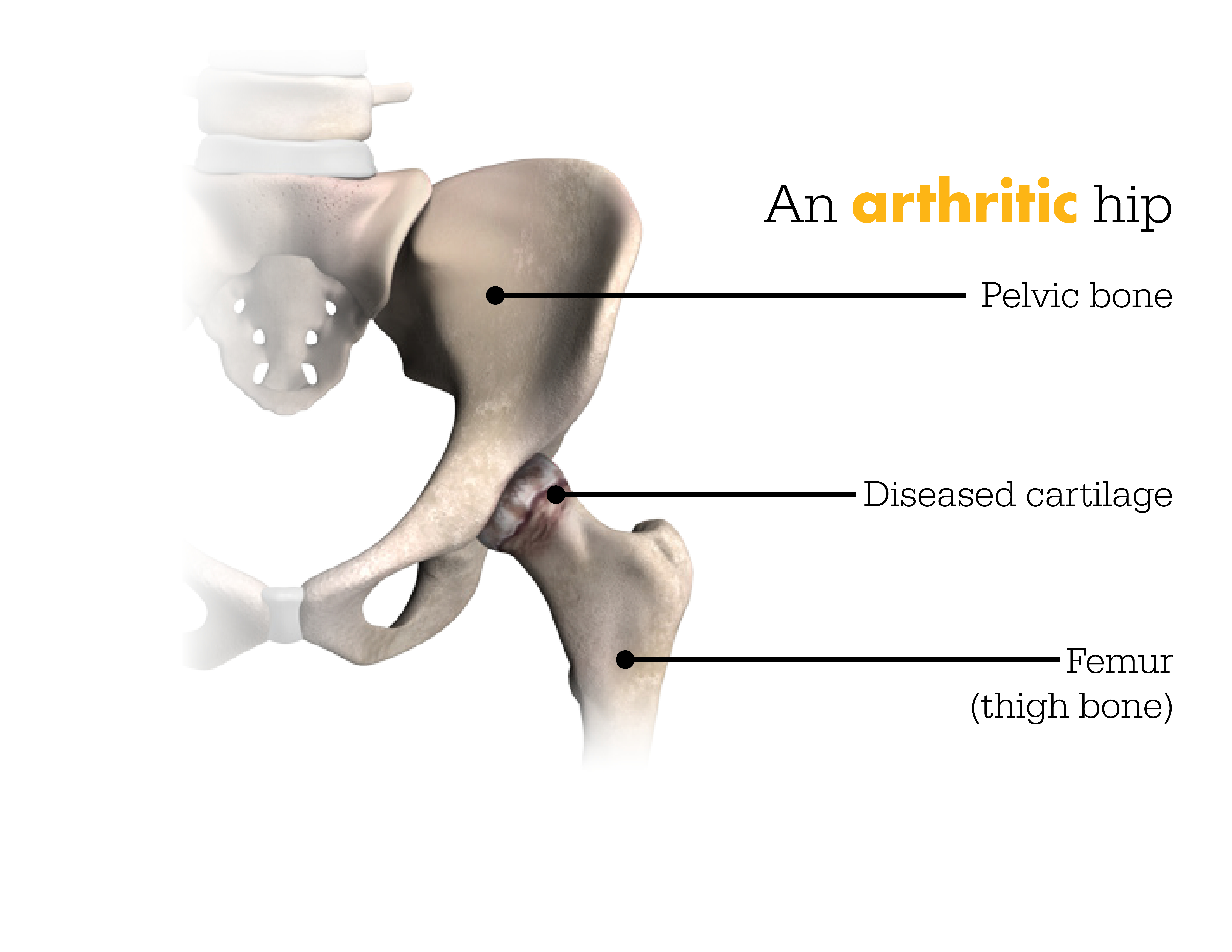
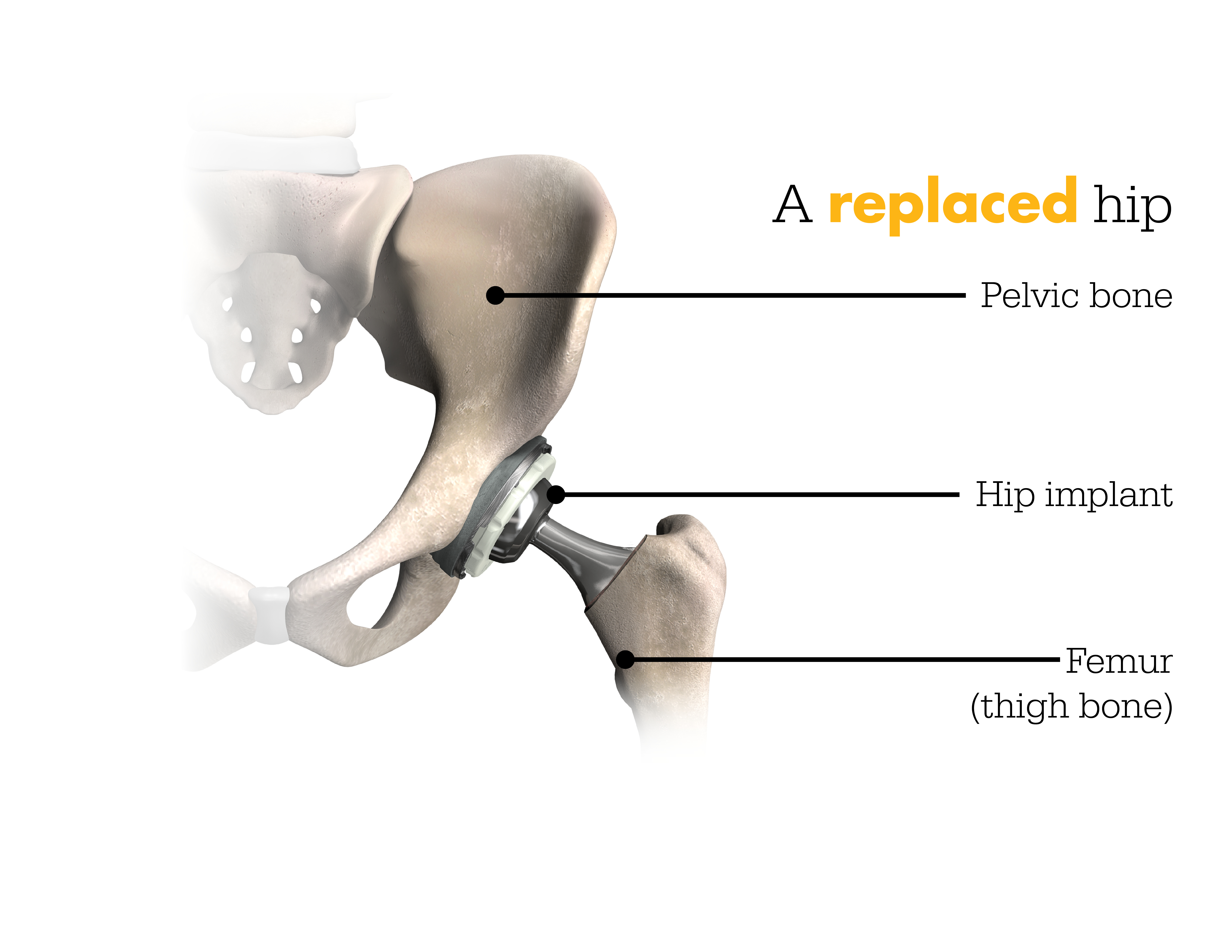
Step 1. Hip CT Scan
Step 2. Hip Personalized Planning

It’s important to understand that the surgery is performed by an orthopaedic surgeon, who guides the surgeon-controlled robotic-arm during the surgery to position the implant in the hip joint. The Mako Robotic-Arm does not perform surgery, make decisions on its own, or move without the surgeon guiding the robotic-arm. The Mako System also allows your surgeon to make adjustments to your plan during surgery as needed.
IMPORTANT INFORMATION
Mako hip replacements
Hip joint replacement is intended for use in individuals with joint disease resulting from degenerative and rheumatoid arthritis, avascular necrosis, fracture of the neck of the femur or functional deformity of the hip.
Joint replacement surgery is not appropriate for patients with certain types of infections, any mental or neuromuscular disorder which would create an unacceptable risk of prosthesis instability, prosthesis fixation failure or complications in postoperative care, compromised bone stock, skeletal immaturity, severe instability of the joint, or excessive body weight.
Like any surgery, joint replacement surgery has serious risks which include, but are not limited to, pain, bone fracture, change in the treated leg length (hip), joint stiffness, hip joint fusion, amputation, peripheral neuropathies (nerve damage), circulatory compromise (including deep vein thrombosis (blood clots in the legs)), genitourinary disorders (including kidney failure), gastrointestinal disorders (including paralytic ileus (loss of intestinal digestive movement)), vascular disorders (including thrombus (blood clots), blood loss, or changes in blood pressure or heart rhythm), bronchopulmonary disorders (including emboli, stroke or pneumonia), heart attack, and death.
Implant related risks which may lead to a revision of the implant include dislocation, loosening, fracture, nerve damage, heterotopic bone formation (abnormal bone growth in tissue), wear of the implant, metal sensitivity, soft tissue imbalance, osteolysis (localized progressive bone loss), audible sounds during motion, and reaction to particle debris.
The information presented is for educational purposes only. Speak to your doctor to decide if joint replacement surgery is appropriate for you. Individual results vary and not all patients will return to the same activity level. The lifetime of any joint replacement is limited and depends on several factors like patient weight and activity level. Your doctor will counsel you about strategies to potentially prolong the lifetime of the device, including avoiding high-impact activities, such as running, as well as maintaining a healthy weight. It is important to closely follow your physician’s instructions regarding post-surgery activity, treatment and follow-up care. Ask your doctor if robotic-arm assisted surgery is right for you.
Stryker Corporation or its other divisions or other corporate affiliated entities own, use or have applied for the following trademarks or service marks: Mako, Stryker. All other trademarks are trademarks of their respected owners or holders.
References
Nawabi DH, Conditt MA, Ranawat AS, Dunbar NJ, Jones J, Banks SA, Padgett DE. Haptically guided robotic technology in total hip arthroplasty - a cadaver investigation. Proc Inst Mech Eng H. 2013 Mar22 7(3):302-9
Illgen R. Robotic assisted total hip arthroplasty improves accuracy and clinical outcome compared with manual technique. 44th Annual Advances in Arthroplasty Course. October 7-10, 2014, Cambridge, MA.F
MKOHMT-PE-3_Rev-1_13841
Copyright © 2017 Stryker CorporationTotal Hip Replacement (THR)
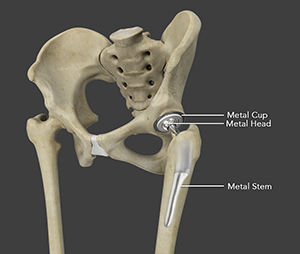
Total hip replacement is a surgical procedure in which the damaged cartilage and bone is removed from the hip joint and replaced with artificial components. The hip joint is one of the body's largest weight-bearing joints, located between the thigh bone (femur) and the pelvis (acetabulum). It is a ball and socket joint in which the head of the femur is the ball and the pelvic acetabulum forms the socket. The joint surface is covered by a smooth articular cartilage which acts as a cushion and enables smooth movements of the joint.
Several diseases and conditions can cause damage to the articular cartilage. Total hip replacement surgery is an option to relieve severe arthritis pain that limits your daily activities.Disease Overview
Arthritis is inflammation of the joints resulting in pain, swelling, stiffness and limited movement. Hip arthritis is a common cause of chronic hip pain and disability. The three most common types of arthritis that affect the hip are:
Osteoarthritis: It is characterized by progressive wearing away of the cartilage of the joint. As the protective cartilage wears down, the bone ends rub against each other and cause pain in the hip. Rheumatoid arthritis: This is an autoimmune disease in which the tissue lining the joint (synovium) becomes inflamed, resulting in the production of excessive joint fluid (synovial fluid). This leads to loss of cartilage causing pain and stiffness.
Traumatic arthritis: This is a type of arthritis resulting from a hip injury or fracture. Such injuries can damage the cartilage and cause hip pain and stiffness over a period.Symptoms
The most common symptom of hip arthritis is joint pain and stiffness resulting in limited range of motion. Vigorous activity can increase the pain and stiffness which may cause limping while walking.
Diagnosis
Diagnosis is made by evaluating medical history, physical examination and X-rays.
Surgical Procedure
Surgery may be recommended, if conservative treatment options such as anti-inflammatory medications and physical therapy do not relieve the symptoms.
The surgery is performed under general anesthesia. During the procedure, a surgical cut is made over the hip to expose the hip joint and the femur is dislocated from the acetabulum. The surface of the socket is cleaned and the damaged or arthritic bone is removed using a reamer. The acetabular component is inserted into the socket using screws or occasionally bone cement. A liner made of plastic, ceramic or metal is placed inside the acetabular component. The femur or thigh bone is then prepared by removing the arthritic bone using special instruments, to exactly fit the new metal femoral component. The femoral component is then inserted to the femur either by a press fit or using bone cement. Then the femoral head component made of metal or ceramic is placed on the femoral stem. All the new parts are secured in place using special cement. The muscles and tendons around the new joint are repaired and the incision is closed.Post-operative care
After undergoing total hip replacement, you must take special care to prevent the new joint from dislocating and to ensure proper healing. Some of the common precautions to be taken include:
- Avoid combined movement of bending your hip and turning your foot inwards
- Keep a pillow between your legs while sleeping for 6 weeks
- Never cross your legs and bend your hips past a right angle (90)
- Avoid sitting on low chairs
- Avoid bending down to pick up things, instead a grabber can be used to do so
- Use an elevated toilet seat
Risks
As with any major surgical procedure, there are certain potential risks and complications involved with total hip replacement surgery. The possible complications after total hip replacement include:
- Infection
- Dislocation
- Fracture of the femur or pelvis
- Injury to nerves or blood vessels
- Formation of blood clots in the leg veins
- Leg length inequality
- Hip prosthesis may wear out
- Failure to relieve pain
- Scar formation
- Pressure sores
Total hip replacement is one of the most successful orthopedic procedures performed for patients with hip arthritis. This procedure can relieve pain, restore function, improve your movements at work and play, and provide you with a better quality of life.
Computer Navigated Surgery
Computer navigation technique is the latest revolution in orthopedic surgery. This technology is used for replacement of arthritic joint.
Computer navigation provides the surgeon with the real time 3-D images of the mapped patients affected joint and the surgical instruments during surgery. The data for the images is provided by the infrared sensors fixed to the bones of the joint and the surgical instruments. Their position is tracked by an infrared camera placed above the surgical table connected to the computer. The computer than generates the real-time images with the help of the appropriate software to guide the surgeon to precisely resurface and cut the bones of the joint and fix the implant precisely & accurately according to the pre-operative surgical plan. Thus, the surgery is done by the surgeon only. Computer navigation is just a tool to guide the surgeon and improve the outcome of the surgery. It cannot replace the skills of an experienced surgeon.
The life of the implant can be extended by precise alignment of the implant and this can be achieved using computer navigation for total joint replacement surgery.Direct Anterior Hip Replacement

Anterior Hip Replacement is a minimally invasive, muscle sparing surgery using an alternative approach to traditional hip replacement surgery. Traditionally, the surgeon makes the hip incision laterally, on the side of the hip, or posteriorly, at the back of the hip. Both approaches involve cutting major muscles to access the hip joint. With the anterior approach, the incision is made in front of the hip enabling the surgeon to access the hip joint without cutting any muscles. A special operating table is used that facilitates various anatomical positions enabling the surgeon to replace the hip joint anteriorly.
Potential benefits of anterior hip replacement compared to the traditional hip replacement surgery, may include the following:- Smaller incision
- Minimal soft tissue trauma
- Reduced post op pain
- Less blood loss
- Shorter surgical time
- Faster healing time
- Less scarring
- Earlier mobilization
- Less post-operative restrictions
- Reduced hip dislocations
- Decreased hospital stay
Normally, after a traditional hip replacement, your surgeon would give you instructions on hip precautions to prevent dislocating the new joint. Hip precautions are very restrictive and usually include the following:
- Avoid the combined movement of bending your hip and turning in your foot.
- You should sleep with a pillow between your legs for 6 weeks.
- Avoid crossing your legs and bending your hip past a right angle.
- Avoid low chairs.
- Avoid bending over to pick things up. Grabbers are helpful as are shoe horns or slip on shoes.
- An elevated toilet seat should be used.
For Anterior Hip Replacement patients, however, hip precautions are unnecessary. Because the muscles are not cut, the risk of dislocation is greatly lessened enabling the patient much more freedom of movement after surgery. Rehabilitation is much faster for patients as well due to less muscle trauma during the surgery.
-
Sports Medicine
- Sports Medicine
- Shoulder Arthroscopy
- Rotator Cuff Repair
- Anterior Cruciate Ligament ACL Reconstruction
Sports Medicine
Sports injuries occur when playing indoor or outdoor sports or while exercising. Sports injuries can result from accidents, inadequate training, improper use of protective devices, or insufficient stretching or warm-up exercises. The most common sports injuries are sprains and strains, fractures, and dislocations.
The most common treatment recommended for injury is rest, ice, compression and elevation (RICE).- Rest: Avoid activities that may cause injury.
- Ice: Ice packs can be applied to the injured area which will help to diminish swelling and pain. Ice should be applied over a towel to the affected area for 15-20 minutes four times a day for several days. Never place ice directly over the skin.
- Compression: Compression of the injured area helps to reduce swelling. Elastic wraps, air casts, and splints can accomplish this.
- Elevation: Elevate the injured part above heart level to reduce swelling and pain.
Some of the measures that are followed to prevent sports related injuries include:
- Follow an exercise program to strengthen the muscles
- Gradually increase your exercise level and avoid overdoing the exercise
- Ensure that you wear properly-fitted protective gear such as elbow guards, eye gear, facemasks, mouth guards, and pads, comfortable clothes, and athletic shoes before playing any sports activity which will help to reduce the chances of injury
- Make sure that you follow warm up and cool down exercises before and after sports activity. Exercises will help to stretch the muscles, increase flexibility, and reduce soft tissue injuries
- Avoid exercising immediately after eating a large meal
- Maintain a healthy diet which will nourish the muscles
- Avoid playing when you are injured or tired. Take a break for some time after playing
- Learn all the rules of the game you are participating in
- Ensure that you are physically fit to play the sport
Some of the common sports injuries include:
Hip Injuries
Fractures of the femur bone, labral tear and hip dislocation are some of the common sports injuries affecting the hip. Hip joint bears more weight and is more susceptible for injuries while playing sports. Hip injuries require immediate medical intervention to avoid further complications. Rehabilitation programs and physical therapy is often recommended following the medical intervention where you need to perform certain exercises to strengthen the muscles and improve the movements.
Read moreKnee Injuries
Anterior cruciate ligament (ACL) is major stabilizing ligament in the knee which may tear with over use of knee for playing sports. The ACL has poor ability to heal and may cause instability. Other common sports injuries in knee are cartilage damage and meniscal tear. Knee injuries of sports may require surgical intervention that can be performed using open surgical or minimally invasive technique. Your surgeon will recommend you for physical therapy to strengthen your muscles, improve elasticity and improve the movements of the bones and joints.
Read moreFoot and ankle Injuries
Foot and ankle injuries include the injuries in the leg below the knee and they are common while playing sports such as football, hockey, skating and in athletes. Treatment for some of these conditions may be orthotics, braces, physical therapy, injections or surgery. Common sports injuries include sprains and strains, ankle fractures, and Achilles tendinitis.
Shoulder Injuries
Severe pain in shoulders while playing your favorite sports such as tennis, basketball and gymnastics may be because of torn ligament in shoulder or shoulder dislocation. These may be caused by overuse of shoulder while playing sports. Simple pain or acute injuries may be treated with conservative treatment and chronic injuries may require surgical treatment.
Shoulder Arthroscopy
Arthroscopy is a minimally invasive diagnostic and surgical procedure performed for joint problems. Shoulder arthroscopy is performed using a pencil-sized instrument called an Arthroscope. The arthroscope consists of a light system and camera to project images to a computer screen for your surgeon to view the surgical site. Arthroscopy is used to treat disease conditions and injuries involving the bones, cartilage, tendons, ligaments, and muscles of the shoulder joint.
Disease Overview
The shoulder joint is made up of a ball and socket joint, where the head of the humerus (upper arm bone) articulates with the socket of the scapula (shoulder blade) called the glenoid. The two articulating surfaces of the bones are covered with cartilage, which prevents friction between the moving bones enabling smooth movement. Tendons and ligaments around the shoulder joint provide strength and stability to the joint. Injury and disease to the bones or soft tissues of the shoulder joint can make it instable, and lead to pain, inflammation and reduced mobility.
Indications
Shoulder arthroscopy is indicated to treat the following shoulder conditions when conservative treatment such as medication and therapy fails to relieve pain and disability:
Shoulder Impingement: this occurs when the shoulder blade applies pressure on the underlying soft tissues when the arm is lifted- Rotator cuff tear
- Frozen shoulder or stiffness of the shoulder joint
- Shoulder Instability this occurs when the head of the upper arm bone slips out of the socket of the shoulder blade’s glenoid cavity either due to injury or overuse
- Biceps rupture occurs when the tendons attaching the bicep muscle to the shoulder or elbow tears
- Damaged cartilage or ligaments
- Bone spurs or bony projections
- Arthritis of the collarbone
Procedure
Your surgeon performs shoulder arthroscopy under general or regional anesthesia. You may be positioned lying down on your side with your arm propped up or sitting in a semi-seated position. Sterile fluid is injected into the shoulder joint to expand the surgical area so your surgeon has a clear view of the damage and room to work. A button-sized hole is made in the shoulder and the arthroscope is inserted. Your surgeon can view images captured by the camera in the arthroscope on a large monitor. Surgical instruments are introduced into the joint through separate small holes to remove and repair the damage to the joint. After surgery, the instruments are removed and the incisions are closed with stitches or small sterile bandage strips.
Post-operative Care
After the surgery, the small surgical wounds take a few days to heal and the surgical dressing is replaced by simple Band-Aids. The recovery time depends on the type and extent of problem for which the procedure was performed. Pain medications are prescribed to keep you comfortable. The arm of the affected shoulder is placed in a sling for a short period as recommended by your doctor. Physical therapy is advised to improve shoulder mobility and strength after the surgery.
Advantages
The advantages of arthroscopy compared to open surgery with a large incision include
- Less pain
- Fewer complications
- Shorter hospital stay
- Faster recovery
Risks and complications
Complications of shoulder arthroscopy include infection, bleeding, damage to nearby nerves or blood vessels, or delayed healing after the surgery. In certain cases, stiffness of the shoulder joint may occur after the surgery. It is important to participate actively in your physical therapy to prevent this from occurring.
Rotator Cuff Repair
Rotator cuff is the group of tendons in the shoulder joint providing support and enabling wider range of motion. Major injury to these tendons may result in tear of these tendons and the condition is called as rotator cuff tear. It is one of the most common causes of shoulder pain in middle aged adults and older individuals. It may occur with repeated use of arm for overhead activities, while playing sports or during motor accidents. Rotator cuff tear causes severe pain, weakness of the arm, and crackling sensation on moving shoulder in certain positions. There may be stiffness, swelling, loss of movements, and tenderness in the front of the shoulder.
Repair
Rotator cuff tear is best viewed on magnetic resonance imaging. Symptomatic relief may be obtained with conservative treatments – rest, shoulder sling, pain medications, steroidal injections and certain exercises. However, surgery is required to fix the tendon back to the shoulder bone. Rotator cuff repair may be performed by open surgery or arthroscopic procedure.
Surgery to repair the rotator cuff has traditionally been done through a large shoulder incision, about 6-10 cm long, and the muscle over the rotator cuff was separated. Newer, advanced surgical techniques have been developed to minimize pain and recovery time. Arthroscopic rotator cuff repair is a minimally invasive surgery performed through tiny incisions, about 1 cm each, with an arthroscope. In arthroscopy procedure space for rotator cuff tendons will be increased and the cuff tear is repaired using suture anchors. These anchor sutures help in attaching the tendons to the shoulder bone. Following the surgery, you may be advised to practice motion and strengthening exercises.
The arthroscope is a small fiber-optic viewing instrument made up of a tiny lens, light source and video camera. The surgical instruments used in arthroscopic surgery are very small (only 3 or 4 mm in diameter) but appear much larger when viewed through an arthroscope.
The television camera attached to the arthroscope displays the image of the joint on a television screen, allowing the surgeon to look throughout the shoulder-at cartilage, ligaments, and the rotator cuff. The surgeon can determine the amount or type of injury, and then repair or correct the problem.
The benefits of arthroscopy compared to the alternative, open shoulder surgery, include:- Smaller incisions
- Minimal soft tissue trauma
- Less pain
- Faster healing time
- Lower infection rate
- Less scarring
- Earlier mobilization
- Usually performed as outpatient day surgery
-
Joint Restoration
Joint Restoration
A joint is a location that connects two or more bones together. It provides support and helps in movement of the knee, hip, elbow, or shoulder. A diseased or injured joint results in joint pain and interferes with the joint movement. Osteoarthritis, rheumatoid arthritis, bursitis, strains, sprains, and other injuries usually lead to painful joints, stiffness, and swelling. Hence, joint restoration becomes essential to repair injured joints, reduce the progression of arthritis, and restore the joints’ original functions.
Joint restoration initially consists of a conservative approach to relieve pain and promote healing. The conservative therapy includes rest, modifying activities, physical therapy, and medications. However, surgery may be essential for those who do not benefit from the non-surgical treatment. Surgery may involve joint reconstruction or joint replacement.Joint Reconstruction
Joint reconstruction includes procedures ranging from minor joint repairs to total joint replacement. The type of joint reconstructive procedure is chosen based on the severity of your joint disorder. Various surgical procedures for joint reconstruction include cartilage restoration, ligament and tendon repair, osteotomy, joint resurfacing and total joint replacement.
- Osteotomy: Osteotomy (cutting of the bone) is performed when the knee joint has been damaged due to the presence of early-stage osteoarthritis. The osteotomy procedure shifts the weight off from the damaged part of the joint and relieves pain. This also helps in increasing the function of the arthritic knee.
- Tendon repair: Suture anchors are used to sew the tendons to the kneecap. This technique brings back the original functions of the joint and its surrounding tissues.
- Resurfacing surgery: Hip resurfacing involves replacing and capping of the damaged hip ball with a metal prosthesis. It does not involve complete replacement of the hip ball. It is recommended for younger patients and has lower chances of dislocation as compared to total hip replacement.
Joint Replacement
Joint replacement involves replacing a damaged joint with an artificial one. This procedure replaces only the damaged parts of joint instead of a complete joint replacement. The prosthesis used as a new joint can be either plastic, metal or both. The prosthesis can be cemented or non-cemented or both methods can be combined together to keep the joint in place.
A minimally invasive joint replacement surgery is performed through smaller, less-invasive approaches. This approach prevents disruption of the surrounding joint muscles and soft-tissues. The minimally invasive approach has advantages of less muscle dissection, minimal pain, quick recovery, and faster rehabilitation.
Patient Info
-
Patient Forms
Patient Forms
With the increasing complexity of necessary medical information compliance, a medical assistant will be assigned to work with each patient to enter necessary medical facts and insurance information in your medical file. This process will take 15-25 minutes at your first visit. To expedite this process please bring a list of medications and be prepared to answer questions about your medical history As a courtesy to the patient, the staff will file insurance claims with your medical insurance company. The business office staff is available to you to answer any questions regarding your policy or office charges.
-
Preparing for Surgery & Procedure
Preparing for Surgery & Procedure
Preparing for Surgery
Once you and your doctor decide that surgery will help you, you will need to learn what to expect from the surgery and create a treatment plan for the best results afterward. Preparing mentally and physically for surgery is an important step toward a successful result. Understanding the process and your role in it will help you recover more quickly and have fewer problems.
Working with Your Doctor
Before surgery, your doctor will perform a complete physical examination to make sure you don’t have any conditions that could interfere with the surgery or the outcomes. Routine tests, such as blood tests and X-rays, are usually performed a week before any major surgery.
- Discuss any medications you are taking with your doctor and your family physician to see which ones you should stop taking before surgery
- Discuss with your doctor about options for preparing for potential blood replacement, includes donating your own blood, medical interventions and other treatments, prior to surgery
- If you are overweight, losing weight before surgery will help decrease the stress you place on your new joint. However, you should not diet during the month before your surgery
- If you are taking aspirin or anti-inflammatory medications or warfarin or any drugs that increase the risk of bleeding you will need to stop taking them one week before surgery to minimize bleeding
- If you smoke, you should stop or cut down to reduce your surgery risks and improve your recovery
- Have any tooth, gum, bladder or bowel problems treated before surgery to reduce the risk of infection later
- Eat a well-balanced diet, supplemented by a daily multivitamin with iron
- Report any infections to your surgeon. Surgery cannot be performed until all infections have cleared up
- Arrange for someone to help out with everyday tasks like cooking, shopping and laundry
- Put items that you use often within easy reach before surgery so you won’t have to reach and bend as often
- Remove all loose carpets and tape down electrical cords to avoid falls
- Make sure you have a stable chair with a firm seat cushion, a firm back and two arms
Preparing for Procedure
If you are having day surgery, remember the following:
- Have someone available to take you home, you will not be able to drive for at least 24 hours
- Do not drink or eat anything in the car on the trip home
- The combination of anesthesia, food, and car motion can quite often cause nausea or vomiting. After arriving home, wait until you are hungry before trying to eat. Begin with a light meal and try to avoid greasy food for the first 24 hours
- If you had surgery on an extremity (leg, knee, hand or elbow), keep that extremity elevated and use ice as directed. This will help decrease swelling and pain
- Take your pain medicine as directed. Begin the pain medicine as you start getting uncomfortable, but before you are in severe pain. If you wait to take your pain medication until the pain is severe, you will have more difficulty in controlling the pain
-
Post-Op Instructions
Post-Op Instructions
Apart from the specific instructions given to you depending on the type of surgery you have undergone, the basic general instructions that you should follow after your surgery are as follows:
- Take pain relieving and other medications as advised. Pain relieving medication should be taken with food. After the first 48 hours of surgery, take the pain medication only when needed.
- Do not drink alcohol, drive a vehicle, operate any machinery or sign a legal document for the first 24 hours after the surgery as the effect of the sedative and/ or the anaesthesia administered during the surgery may last for the first 24 hours of the surgery.
- Use ice packs to control swelling. However make sure that the ice bag does not leak into the dressing. Ice packs can be used liberally for 2 weeks and even later, if required.
- Follow the specific restriction of activity, as advised. Remember that it is easier to prevent developing pain rather than managing it once it has already developed. Rest for a few days after the surgery and keep the operated extremity elevated, above the level of your heart, to control swelling.
- You will be instructed when the surgical site may be washed briefly with antibacterial soapy wash rag and thoroughly dried and covered with dry gauze and no ointment.
- Dr. Sikes will instruct you when to begin physical therapy. He prefers that you use the therapy team at Southern Bone and Joint for your recovery.
- Eat a healthy diet and drink plenty of non-alcoholic and non-caffeinated drinks.
- Schedule your follow up appointment with your doctor as advised.
Please consult your doctor immediately if you experience any of the following symptoms:
- Increased drainage from the incision
- Increased redness around the operated area
- Increased swelling that does not decrease with ice and elevation
- Foul odor
- Fever greater than 101°F
- Coldness, numbness or blanched white or bluish colour of the fingers or toes
- Sudden calf pain or shortness of breath
- Chest pain
-
Useful Links






